Abstract
Background Infective endocarditis (IE) is defined as pathogen-induced inflammation of the heart valves characterized by local vegetation formation and systemic immune-related phenomena. Patients present with unspecific symptoms such as fever and shortness of breath, and definitive diagnosis is often delayed until local or systemic complications such as valvular destruction, abscess formation or systemic thromboembolisms occur. Despite a mortality of more than 30% within 12 months of diagnosis, therapeutic options remain scarce and pathophysiological understanding of innate and adaptive defense mechanisms in humans is limited.
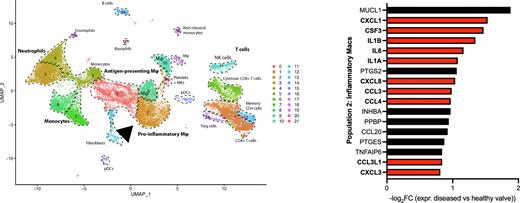
Methods Here, we prospectively enrol patients with acute infective endocarditis according to modified Duke criteria (n=32) to longitudinally profile and immunophenotype systemic immune response at single-cell resolution using transcriptomic profiling (scRNAseq, bulk sequencing) along with proteomics and flow cytometry approaches. We compare blood samples of endocarditis patients with healthy controls (n=45) as well as an independent, prospectively enrolled cohort of patients with acute non-cardiac bacterial infection (n=28), comprising a total of > 100 individuals. In a select subset of patients requiring surgical valve removal, we use CD45-enrichment by flow cytometry and subsequent single-cell sequencing to investigate transcriptomic phenotypes of immune cell populations within healthy and diseased valvular tissue to identify local immune responses to endocarditis. We integrate these data with clinical parameters and plasma proteomics to comprehensively immunophenotype infective endocarditis.
Results IE patients diagnosed by modified Duke criteria exhibited early neutrophilia and leukocytosis that returned to normal values upon antibiotic and surgical treatment, while other leukocyte subsets did not exhibit differential relative abundance compared to healthy controls and patients with extra-cardiac bacterial infection. Neutrophils from endocarditis patients upregulated proinflammatory cytokines and microbicidal factors at protein level, and plasma proteomics revealed an early signature characterized by activation of the complement system, multi-level coagulation factors and antimicrobial S100 proteins. Single-cell sequencing of over 130,000 peripheral mononuclear blood cells (PBMCs) revealed an endocarditis-specific upregulation of immunothrombosis-related, proinflammatory transcription programs across the myeloid and lymphoid cell compartment. In addition, transcriptome analyses of CD45+-sorted cells retrieved from surgically resected infected valves revealed a predominantly monocytic und neutrophilic influx in diseased valves of endocarditis patients. Monocyte/macrophage populations within the valve expressed proinflammatory and neutrophil chemotactic cytokines including CXCL8 and colony-stimulating factor 3 (CSF3), interleukin 6 and interleukin 1beta along with prothrombotic, complement-associated transcripts, aiding in the recruitment of infiltrating leukocytes into vegetations and (para)valvular tissue, promoting a vicious, self-sustaining circle ultimately leading to valvular destruction.
Discussion This study provides a comprehensive and holistic immunophenotyping approach of both local and systemic immune responses to infective endocarditis in humans. For the first time, we provide deep insights into pathogen-induced adaptations in patient-derived resident and circulating immune cells, which may explain the complex clinical picture of endocarditis, and reveal upregulation of immunothrombotic pathways in innate immune cells. These findings may explain to complex interplay between possibly detrimental host responses, prothrombotic phenomena and the causing pathogen. Our study therefore provides a framework for a deeper pathophysiological understanding of infective endocarditis and may aid in the development of both diagnostic and novel therapeutic approaches towards this cryptic and lethal disease.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal